As more regions and jurisdictions develop “End the Epidemic” plans, I am left wondering what happens to us, the community of people living with HIV? How are we participating? Are there spaces for us to have a meaningful voice? How do we mobilize people living with HIV to participate and get our diverse voices and needs heard in these initiatives?
Or are we relying on a few key leaders living with HIV to represent all of us?
Most of the End of the Epidemic plans in the United States focus on four pillars: increasing HIV testing so everyone knows their status, increasing clinical access and usage for both HIV prevention and treatment, and increased surveillance so resources can be directed. While these are laudable goals, I am a little skeptical if these particular programs will end the HIV epidemic.
Let me be clear, I understand the science behind each of these strategies. I get how – in an ideal world – they would operate in a complementary way to reduce HIV transmission and increase HIV health. But I also recognize the limits of these strategies in dealing with our actual lives.
How do these End the Epidemic plans address the structural conditions (e.g. poverty, racism, sexism, homophobia, transphobia, ableism – just to name a few) that made us vulnerable to HIV in the first place?
Treatment will not change these larger structural contexts.
I take my HIV meds daily (unless I forget – it happens!). But I also understand that my HIV meds will not ameliorate financial stress, help with my feelings of social isolation, pay for my therapist, and ensure a livable wage and job security.
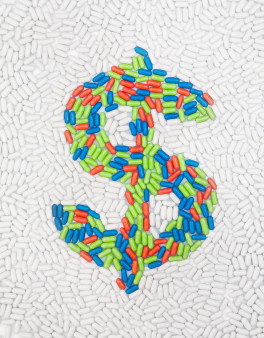
In HIV, we used to understand that we could not separate how people lived with their HIV health outcomes. We fought for housing and Ryan White support services. Now, more and more, it seems we are reduced to people who take pills.
This can change. If the CDC required health departments to meaningfully engage community groups (and funded it), then I could see the End the Epidemic plans that had a chance to succeed. If the health departments reached beyond the few people that sit on various planning councils and permitted these community voices to have real power in decision-making, then there could be some innovative policies and actions.
Instead, I am afraid of the same-old, same-old. Plans with vague HIV testing initiatives, linkage to care services, a few standard HIV prevention behavior change interventions, and an aggressive surveillance system that targets the most marginalized people living with HIV. Plans that are meant to augment health department staffing and infrastructure, and not build up community-led responses.
I know that the End the Epidemic initiatives were a key part of the recent United States Conference on AIDS (USCA). I also know that the health departments and CDC had a one-day institute without community present.
CDC can hold health departments accountable to community engagement. It is a common tactic to require grantees to conduct activities a certain way. CDC has required health departments to conduct names reporting in HIV surveillance, have advisory groups to approve HIV health promotion materials and to implement certain activities as part of their HIV portfolio (such as community planning, HIV testing, surveillance, linkage to care and behavior change interventions). Why can’t CDC provide more robust demands for community engagement?
I am worried that our voices and needs as people living with HIV are reduced to treatment adherence. What about treatment access? Harm reduction and mental health services? Poverty reduction and affordable housing initiatives? Eliminating HIV criminalization laws? Support for immigrants? Sexual and reproductive health and rights?
There was a time when I was homeless in Los Angeles, couch surfing for months. At some point, I stabilized my housing but developed a crystal meth habit. Some of my friends stood by me, accepting that I was erratic, clearly in pain and unable to manage basic interactions sober. I became a client at APLA and the Los Angeles LGBT Center, where I got food and medical services. I refused to take HIV medication in these years, insisting that my health was not declining and scared of side effects such as lipodystrophy. At the time (early 2000s), my clinical care providers understood that HIV treatment was not the biggest issue I faced: they worked with me to make sure I had access to food and harm reduction services.
I bring this up because if my service providers had insisted on HIV treatment, I probably would have stopped going to my appointments. I can look back and imagine that my physicians understood this and adjusted our clinic encounters appropriately. Today, with the clinical guidelines so focused on TREATMENT TREATMENT TREATMENT, I do not know if other people living with HIV with drug use and housing issues are having the same options.
Our issues are broader than our meds. Access and adherence are contingent on a wider context of our lives – our income, our housing, our social support network, and our pain and trauma.
The CDC and health departments cannot “end the epidemic” without the meaningful involvement of people living with HIV. And that means seeing us - and our broad diverse community - as partners in developing, implementing and evaluating the End the Epidemic plans, policies and procedures.







4 Comments
4 Comments