New York City, which has engaged in an aggressive, coordinated, well-funded and multipronged assault against its HIV epidemic in recent years, is thus far making superb progress in its effort to end the virus’s status as a major local public health threat. The city that was once the nation’s main HIV epicenter is celebrating dropping below 2,000 annual diagnoses for the first time.
That said, progress has been slower for certain marginalized populations, including African Americans and transgender individuals.
These and other findings relating to the city’s epidemic were published by the New York City Department of Health and Mental Hygiene (NYC DoHMH) in its 2018 HIV Surveillance Annual Report.
New York’s progress is driven by improved HIV testing, rapid linkage to medical care for those who test positive and a rising rate of viral suppression among those in care. Additionally, pre-exposure prophylaxis (PrEP) is extraordinarily popular among men who have sex with men (MSM) in the city.

A maverick leader in the city’s HIV fight, Demetre Daskalakis, MD, MPH, deputy commissioner for the Division of Disease Control of the New York City Department of Health and Mental Hygiene at his office in 2015Benjamin Ryan
The city saw 1,917 new HIV diagnoses in 2018, an 11% decline from the 2,157 diagnoses in 2017. The estimated annual rate of new infections (as opposed to diagnoses) declined by 16% between 2017 and 2018 and by 41% between 2014 and 2018.

Source: NYC DoHMH

Source: NYC DoHMH

Source: NYC DoHMH
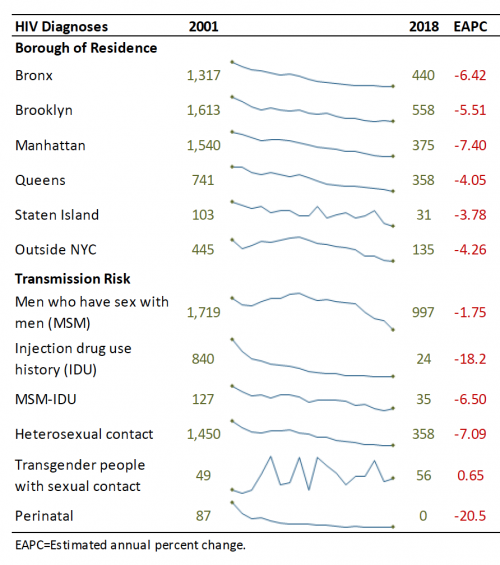
Between 2001 and 2018, new annual diagnoses dropped from 1,719 to 997 (a 41% decline) among MSM, from 840 to 24 (a 97% decline) among people with a history of injection drug use, from 127 to 35 (a 72% decline) among MSM who inject drugs and from 1,450 to 358 (a 75% decline) among heterosexuals. Among transgender people, there were 49 diagnoses in 2001 and 56 in 2018.
Source: NYC DoHMH
For the second time since the city began surveillance of mother-to-child transmission of HIV, no infants were born with the virus in 2018. In 2001, 87 such births occurred.
In 2018, 45.9% of HIV diagnoses were among Blacks, 36.4% were among Latinos, 11.4% were among whites and 5.4% were among Asians.
Since 2017, the number of new diagnoses among men and women, all major racial groups, residents of all of the city’s five boroughs and nearly all age groups declined. Such declines were steepest among men, whites, Asians, people in their 20s, residents of Brooklyn, Queens and Staten Island (the other two boroughs are the Bronx and Manhattan), MSM and people with a history of injection drug use.
Groups that saw an increase in diagnoses between 2017 and 2018 included transgender people, people in their 50s and MSM who inject drugs.
Of the 59 diagnoses among transgender people in 2018, 56 (95%) were among trans women and three (5%) were among trans men. A total of 58% of the diagnoses were among Blacks, 30% were among Latinos and 6.8% were among whites. Sixty-three percent of the diagnoses were among trans people in their 20s. For 95% of the diagnoses, sexual contact was the reported risk factor.

Source: NYC DoHMH
Between 2003 and 2017, the annual rate of death from any cause among people with HIV declined by 65% while the rate of death from HIV-related causes declined by 83%. In 2017, just 28% of deaths among people with HIV were related to the virus.

Source: NYC DoHMH
Eighty-four percent of people diagnosed with HIV in 2018 were linked to medical care for the virus within one month of diagnosis, a 20% increase compared with 2017, when 70% of those diagnosed were linked that fast. Fifty-three percent of those diagnosed in 2018 had a fully suppressed viral load within three months, a doubling of the 26% rate seen in 2014.

Source: NYC DoHMH
Lower proportions of women, transgender people, Blacks and people with a history of injection drugs use were linked to care and virally suppressed soon after diagnosis.
In 2018, 77% of the estimated population of people living with HIV (including those not diagnosed) achieved viral suppression. The report defined viral suppression as having a most-recent viral load test result under 200.

Source: NYC DoHMH
Fewer transgender people, Blacks, Latinos, young people and people with a history of injection drug use had a fully suppressed viral load.
Of those HIV-diagnosed people in medical care for the virus, 87% were virally suppressed in 2018, up from 81% in 2014, a 7% increase. That year, 67% of those in care had a sustained fully suppressed viral load, up from 58% in 2014, a 15% increase. Sustained viral suppression was defined as having at least two viral load tests taken at least 14 months apart with all test results in 2017 and 2018 under 200.
The Centers for Disease Control and Prevention has recently been pushing to look at sustained viral suppression as a better indicator of the overall health of a given HIV population. Looking at only the most recent test result can mask variations in individuals’ viral suppression status over time, as is evident from these New York City figures.

Source: NYC DoHMH
To read the report, click here.







1 Comment
1 Comment