Canadian men who refused a nurse’s offer of pre-exposure prophylaxis (PrEP) against HIV reported various reasons for declining, including not considering themselves at risk for HIV and not thinking they could manage adhering to daily drug regimen, aidsmap reports.
Patrick O’Byrne, RN, PhD, of the School of Nursing at the University of Ottawa, and colleagues studied a program in which nurses offered PrEP to people with risk factors for HIV acquisition. Publishing their findings in AIDS and Behavior, they analyzed responses from individuals who were recommended PrEP between August 2018 and August 2019.
The nurses offered PrEP to people who were diagnosed with syphilis, chlamydia or rectal gonorrhea and to those who had ever taken post-exposure prophylaxis (PEP) or if the nurse deemed them to be at high risk for HIV for another reason.
Of 340 people offered PrEP, 98% were men. About one in four of them were ineligible to take PrEP for medical reasons, such as being HIV positive or already on PrEP or due to problems related to their health insurance.
Of the 261 remaining people included in the analysis, 48% accepted the nurse’s recommendation of PrEP.
“While half our patients declined a referral,” the study authors wrote, “the other half agreed, which we took as a sign of project success because we linked these patients with PrEP when they otherwise would not have.”
Three people in the analysis were ultimately diagnosed with HIV. One person said no to PrEP twice; another accepted the referral for PrEP but never started it; and the third, as testing would reveal, already had HIV when offered PrEP.
All the people who declined PrEP were men. They were 35 years old on average. The lowest rate of declining PrEP was seen among those diagnosed with rectal chlamydia or gonorrhea, at 30%. The highest rate, 55%, was seen among those the nurse judged to be at high risk for HIV.
Most commonly, the men who declined PrEP said they didn’t see themselves as at risk for HIV (42% reported this). Fourteen percent of those who did not opt for PrEP did not think they could manage the prescription, citing their mental health, travel plans and anxieties about costs associated with the prescription.
In the United States, PrEP is widely covered by insurance. Starting in January 2021, federal law will require that all insurers cover PrEP with no cost sharing, such as co-pays or deductible payments, and no preauthorization requirements.
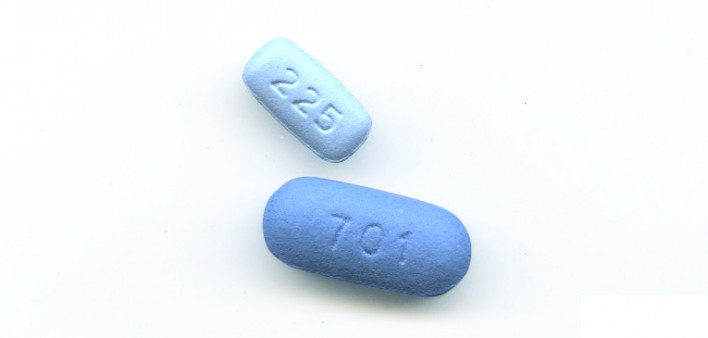
In the meantime, Gilead Sciences, which manufactures Truvada (tenofovir disoproxil fumarate/emtricitabine) and Descovy (tenofovir alafenamide/emtricitabine), the two approved forms of PrEP, provides a co-pay assistance card that covers up to $7,200 in out-of-pocket expenses related to obtaining PrEP, with no monthly limit. For those who are uninsured, Gilead is partnering with the federal government to provide PrEP at no cost.
All this said, the costs associated with the quarterly monitoring required to maintain a PrEP prescription, including clinic visits and HIV, sexually transmitted infection and kidney function tests, are not covered by any of these benefit programs. Such costs are, however, typically covered by insurance.
In the new study, men who rejected the offer of PrEP often cited negative attitudes about the preventive drug. They considered it “harmful” or “toxic” and were worried that they would be stigmatized if others saw them taking PrEP.
Truvada and Descovy are both well-tolerated medications. Compared with Truvada, Descovy is associated with improved biomarkers associated with bone and kidney health. However, to date no evidence has connected the use of Truvada as PrEP with actual kidney disease or bone fractures—two rare outcomes. Nor have researchers determined that using Descovy lowers the risk of such outcomes compared with using Truvada.
The study authors concluded that the considerable proportion of participants who declined PrEP because they didn’t think they were at risk for HIV “highlights the need for more research about people’s perceptions of HIV risk and PrEP, and how, when and why these feel this intervention would be necessary. Considering ongoing HIV transmission, better tailoring PrEP to persons who could benefit [from] it might yield tangible HIV prevention outcomes at the individual and population levels.”
To read the aidsmap article, click here.
To read the study, click here.






1 Comment
1 Comment